Is Your Liver Happy
Exercise is not a game changer for healthy weight loss as much as it is for maintaining a healthy weight. Most of us aren’t having routine blood work that looks at our liver enzymes and even if you are by the time they are elevated your liver has been under insult for a while.
Here we are a month into 2019 and what we knew about health last year remains pretty much the same. For the large majority of people we find a “health lane” and stick to it. For one person that may look like high-activity levels 5-6 days of “training” per week, a Whole 30 eating protocol, 5-day work week at the office, and the occasional cocktail outing with friends. On the other end of the spectrum person “x” eats mostly vegetarian, engages in yoga once a week, prefers snuggling with their cat, and enjoys church activities.
People tend to find their comfort zone and begin habit building from a young age. In many cases adopting practices and ideas from their parents and peer groups. Cue the “my mom and dad had this or that issue, must be my genetic cards,”
However we choose to behave it is altering our bodies and physiology at a cellular level. In some ways, and much like our current healthcare system, these behaviors feel uncoupled from our health trajectories. This is because while some activities (injuries, sleep, caloric consumption, food choice, activity levels etc.) have short-term effects the long-term patterns result in ramifications that trickle out over 5 -20 years before we realize their full effect. Often times it’s very difficult to rule out early stage pathology or disease barring an invasive diagnostic test.
Overtime the body gives back, adapts, based on what has been required of it. As a student of the musculoskeletal system the research is quite clear when it comes to how quickly the neuromuscular complex can refashion itself. The Center for Healthy Aging and the Department of Biomedical Sciences at the University of Copenhagen concluded that it takes two weeks for a young person not using a leg to lose 1/3 of their muscle strength and mass leaving them on par with a person who is 40-50 years their senior.
Inactivity does not discriminate and affects both young and old. What is more interesting is that after 2 weeks of immobilization participants cycle trained 3-4 times per week for six weeks. This was not enough for them to regain their muscle strength unless they included weight training.
This example demonstrates how quickly the body adapts to inactivity and results in rapid muscle loss. The real kicker is that it will take you three times the amount of time to regain the lost muscle mass.
Let’s look at a few examples of disease that require a period of 10-20 years before the disease has fully developed and spill over into other organ systems. Most people don’t realize that cirrhosis of the liver and the deposition of connective tissue (scarring and fibrosis) requires about 80 grams of ethanol daily for 10- 20 years. For those wondering what’s 80 grams - there is roughly 14 grams of ethanol in a 12 oz beer.
More importantly, non-alcoholic fatty liver disease or NAFLD parallels that of obesity and has steadily risen over the last 30 years. NAFLD is projected to become the leading cause of liver related morbidity and mortality within 20 years and a leading indication for liver transplantation in the next few years.
Some researchers are calling diabetes a disease of the liver first. The liver is an important organ especially for energy metabolism and storage. The development of Type 2 Diabetes takes around 5-10 years in adults and can take much less time in children. These are 2 examples of long-term metabolic disorders. Atherosclerosis (think plaque and eventual heart attack) would be another example of inter-related long term metabolic stress that leads to maladaptive changes to an individual’s physiology.
Nutrition in the broader context of caloric intake
If you overload the system with continued doses of “fuel” whether alcoholic beverages, sugar, or fat/protein for that matter, eventually the body will be unable to effectively process, detoxify and utilize these energy sources. A fatty liver is a signal that it is unable to burn fuel appropriately. A healthy liver ranges from 1-3 % fat and once it is at 5% normal function is on the line.
Judging by the statistics, if you’re an American, chances are you may stand to shed a few pounds. This tradeoff, excessive pounds for improved function, will increase your overall health and longevity. I’ve heard firsthand from patients, friends and family how difficult it can be to shed some weight and how to track progress when the scale seems to stall. Even exercise has its limits if your liver is struggling. Exercise is not a game changer for healthy weight loss as much as it is for maintaining a healthy weight.
Most of us aren’t having routine blood work that looks at our liver enzymes, and even if you are by the time they are elevated your liver has been under insult for a while. The only way to rule out fatty liver is with a biopsy. Dr. Alan Christianson shares an interesting statistic: in situations where healthy individuals are undergoing testing to provide liver tissue donation 40.2% were found to have fatty liver disease. These are individuals with otherwise healthy blood markers.
Height to waist ratio
How do I know if my liver is strained or how it is handling the cumulative energy load? One of the most important metrics is your waist circumference. Your waist should be less than ½ your height. If it’s larger you may be more likely to have higher triglycerides, lower HDL cholesterol, higher LDL particle size, elevated inflammatory markers, elevated blood pressure, and higher fasting glucose.
If you want to quantify your risk of fatty liver disease Dr. Christianson has a built a calculator (because, as we know, short of a biopsy every other marker is inherently imperfect).
Fatty Liver Index
All you need are some results and some measurements:
The measurements you need:
Weight in pounds
Height in inches
Waist circumference in inches
The blood test results you will need:
Fasting triglycerides
Fasting GGT
Unlike your car, your liver doesn’t want to be “topped off” at every meal. Whenever we eat above and beyond our basal fuel requirements metabolic processes result in elevated free radicals and inflammatory compounds. Energy production is a “dirty process” metabolically speaking and requires the liver to run it’s detoxification pathways.
Trust me, the body is not trying to carry trapped fat around our midsection. If you give the liver no choice and subject it to fuel overload this will result in high density fat storage, high blood glucose aka pre-diabetes/diabetes type 2, suppressed metabolism, and increased levels of pro-inflammatory adipokines.
In addition to eating nutrient dense meats, dairy, fruits and vegetables, do I take any evidence-based supplements for liver health?
Liver specific support
N- Acetyl-L - Cysteine: can raise the liver’s protective glutathione
Milk thistle: shown to protect liver cells and safeguard it from cell death
Alpha lipoic acid, Taurine, and Betaine Anhydrous
Dandelion tea to enhance bowel secretion and liver function
Health care solutions when you have decided to stop chasing symptoms.
Instead of giving Amy steroids indefinitely to control her eczema, the conventional method of treating eczema, we’re taking steps to heal her by identifying and treating the root cause.
As a Functional Medicine nutritionist, I think like a detective to help my clients understand the "why" behind their "what" (the diagnosis). Sometimes, the "why" can be revealed in a simple conversation; more often, more investigation is needed (various types of functional testing and lab work).
The following is an example of one hunt for the root cause of a client's problem. It was a simple conversation over dinner. Amy showed me the dry itchy patches on her hands, which I recognized as eczema, the "what" or diagnosis. To really help Amy and keep her away from the stereo typical treatment with cortisone cream, I now needed to know the "why."
Me: How long have you had the itchy dry spots?
Amy: A couple of months
Me: Are you prone to UTI’s or yeast infections?
Amy: I had my first yeast infection a month ago.
My thoughts are that two things are happening within a month of each other, both possibly stemming from gut imbalances.
Me: Have you had a round of antibiotics within the last 6 months?
Amy: No
Me: Are you taking birth control pills?
Amy: Yes
Me: For how long?
Amy: 3 months
BINGO! Birth control pills are notorious for altering gut bacteria. We’d found the smoking gun, the "why."
I already knew that Amy had a history of chronic constipation as well as acne. Before starting the pill, she likely had bacterial imbalances and the BC pills triggered the eczema, which always has its origin in the gut.
Since she wasn’t ready to stop the birth control pills, the best path was to find ways to support her gut flora so that together, her acne, constipation, yeast and eczema would subside.
I recommended cutting out all dairy and adding probiotics and non-dairy fermented foods. For further support, I suggested 50 mg B6, in the absorbable form of pyridoxal -5- phosphate as BC pills deplete B6 (a vitamin that influences energy, metabolism and the formation of neurotransmitters, influencing sleep, anxiety and depression). Lastly, I recommended vitamin D to help modulate the immune system.
If these steps do not give us the results we expect to see within a couple months, I’ll recommend a stool test to determine the function of her digestion and to rule out any parasites or pathogenic bacteria.
Instead of giving Amy steroids indefinitely to control her eczema, the conventional method of treating eczema, we’re taking steps to heal her by identifying and treating the root cause.
To read more about gut health and bacteria click here. https://alivingbalance.net/2015/05/invitation-to-a-digestion-party/
Written by: Cindy Dupuie, CN
Edited by: Vicki Ronaldson
www.alivingbalance.net
SATURATED FAT & CHOLESTEROL: THE HEART DISEASE SCAPE GOAT ( Part 3)
At the core of any diet there are two fundamental truths when it comes to eating for your health.
Number 1: Avoid processed and refined food
Number 2: Choose nutrient dense foods and incorporate healthy/traditional fats
What does PUMP mean?
Welcome Back! Continuing from part 2. Now we are going to build on the basic info and screening tools. We’ll touch on the more advanced markers to help stratify an individual’s risk for cardiovascular disease. Remember these tests are not bulletproof data points. It’s not a black and white process. A thorough history, review of systems and specific health assessment measures can provide a great blueprint.
Plates not Pills
Armed with that information patients may take the necessary dietary and lifestyle changes to improve how they feel, decrease negative symptoms and see blood markers normalize. You would be hard pressed to find doctors that would deny lifestyle modification as the primary form of intervention. It’s always a good idea to consult with your physician to discuss medication and track your overall heart health.
Useful markers/tests for determining cardiovascular risk
* Included in an Iron panel: serum iron, TIBC, UIBC iron saturation aka transferrin saturation
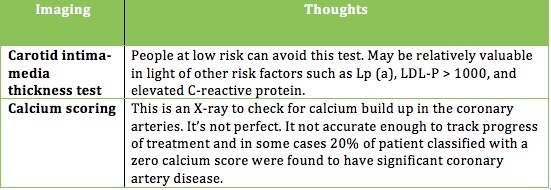
Two Additional tests that some physicians utilize.
Without a needle or Imaging
If you’re inclined you may want to use one of these two online calculators to give you a basic sense of your risk for heart disease.
If you are over twenty years of age and do not have heart disease or diabetes you can calculate your risk using the Framingham 10-year Risk Calculator. The inputs include: age, gender, total and HDL cholesterol, smoking status, and blood pressure. The Reynolds Risk score might be a better option. It includes family history and C-reactive protein.
If you are ready to minimize your risk, limit your medications and learn what makes up a heart-healthy action plan read on.
In the spirit of heart health
I’ve come up with a mnemonic to help you understand the right approach. PUMP
P - purposeful eating
U - understand your risk
M - measure to be sure
P – participation and lifestyle modification
Over the course of these 3 articles we’ve brushed up on the 3-legged stool of heart disease: (1) why it happens, (2) what causes it, and (3) what’s your risk. Let’s talk about the seat of the stool as it holds all of the legs together and acts as the cornerstone. In this analogy the seat can be divided into 3 parts: Diet, weight management, and exercise.
If you are overweight and want to reduce your risk of heart disease without the side effects of medication eating with purpose will help you lose the weight. Improving one’s relationship with food must be tailored to the individual.
At the core of any diet there are two fundamental truths when it comes to eating for your health.
Number 1: Avoid processed and refined food
Number 2: Choose nutrient dense foods and incorporate healthy/traditional fats
Why? Eating this way curbs inflammation, hunger, weight gain, and metabolic syndrome (recall 1/3 Americans are estimated to have MetS).
From a bird’s-eye view the majority of food should come in the form of meat, poultry, fish and shellfish, non-starchy vegetables, starchy tubers, fruit, nuts, and seeds. Sorry guys please don't try and find these items at Olive Garden or Taco bell.
If you are currently floundering on the standard American diet (SAD) this may feel a bit like an elimination diet. How many daily grams of carbs does the average American eat? Take a guess. It’s around 300 to 400 grams of carbs per day! Delicious, I know. However, the lion’s share comes from refined carbohydrates such as breads, cereals, chips, pasta and crackers. A more sensible target, utilizing whole foods, puts one at 50 - 250 grams of carbs per day. So you’re wondering — Is he suggesting that I go on a plant-based, keto, paleo, or an atkins-like diet? Can I drink milk and eat pizza and pasta?
I am suggesting some form of a modified paleo-ish diet. As for dairy it’s best to eliminate for one month and add it back in to see how it’s tolerated. Eliminating grains entirely may be a hard sell, but you won’t know how you feel or how you’re body will change if you don't give it shot. It doesn’t get much attention, but grains contain certain anti-nutrients that can cause digestive problems and other stealth health issues.
Let’s talk turkey (of the sea)
The average American eats a ratio of anywhere from 12:1 to 25:1 Omega 6 to omega 3 fatty acids. This creates a highly inflammatory state. Usher in some cold-water fish. Some studies suggest that eating 8 oz of fish / week (we’re not talking tilapia; it’s farmed and high in omega 6) would equate to 20,000 few deaths from CVD and 4,000 fewer nonfatal strokes. It’s been speculated that regular fish consumption may reduce total mortality at a higher rate then statins (statins garner 40 billion dollars a year and is a article in itself).
So if not tilapia? We want fish high in omega 3 such as salmon, mackerel, herring, sardines, anchovies, and bass, as well as shellfish like oysters and mussels. The single highest seafood source of EPA and DHA is caviar or fish eggs. I could not eat fish eggs if my life depended on, but if you like them more power to you.
If you want to hit a clinically relevant range of omega 3’s you want to eat 3.5 EPA plus DHA per week. This may reduce heart disease by as much as 25%. A good goal would be to eat between 10-16 oz of fatty fish/shellfish per week. Make up any short fall with a high quality fish oil supplement.
When it comes to other healthy fats olives, olive oil avocados, and macadamia nuts provide healthy monounsaturated fats. Remember monounsaturated fats have been shown to reduce LDL and Triglycerides, decrease oxidized LDL, lower blood pressure, decrease thrombosis, and reduce incidence of heart disease.
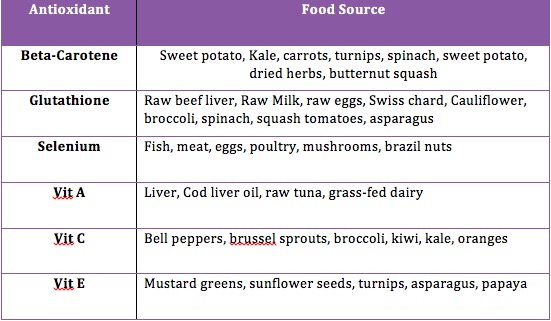
You might be familiar with the term antioxidants. If you recall shortages in antioxidants may contribute to an increase in oxidized LDL, which is associated with arterial plaque build up. Food companies do an excellent job with their packaging to seduce the consumer. The supplement and nutraceutical industry is vying for you to seek out their pills. While supplements may be beneficial in some situations, it’s preferable to get these nutrients we need from whole foods, Mother Nature, and not isolated synthetic sources like ascorbic acid.
There is mixed support in the medical literature on antioxidant supplementation. You may have heard that treatment with beta-carotene, vitamin A and vitamin E may increase mortality. For reasons we that have not been fully discovered whole foods appear to be more effective than supplements in meeting nutrient requirements.
Foods high in antioxidants (lower oxidative stress and inflammation) include leafy greens and berries, but there is more to the story. Red meat and organ meats are also rich in antioxidants that are not found in significant amounts in plant sources.
I don’t want to go any deeper into the nutritional weeds. Remember there is no one-size fits all approach. Ultimately, a heart healthy diet requires some attention. It starts by eliminating processed foods and switching to nutrient dense whole foods. There should be an emphasis on cold-water fatty fish and shellfish, healthy fats, antioxidants rich foods, polyphenol-rich foods, soluble fiber, nuts, fermented foods and occasional alcohol. If you decide to supplement be selective. For example, it’s better to take folate then the synthetic folic acid. Much of folic acid is never converted to folate.
Back to the stool analogy
Earlier I broke the stool seat into 3 parts, diet, weight management, and exercise. For most people combining diet and exercise will help you reclaim a healthy weight. The evidence is pretty straightforward and suggests that regular moderate exercise prevents the build up of arterial plaque, improves lipids and reduces vascular symptoms in people with heart disease. Exercise is a great way to reduce stress, and you may have heard me cite stats on the interplay of stress and risk of cardiovascular disease. I’m not proposing everyone flock to the nearest HIIT gym or LA fitness. Make small changes based on your current activity level and attempt to log 10,000 steps a day.
Questions
If you have any specific questions regarding this 3-part educational series (testing, supplementation, lowering high blood pressure, or statin drugs) please contact me at nick @spineandjointoc.com
Emotional Vulnerability: Take care of your body to take care of your mind
The holidays can mean different things for each individual. Some thrive, others stress about cooking, traveling, gift giving, and perhaps overeating. It’s also a time most of us begin to turn the page on the current year looking to the future. Here is short piece on how to groom your emotions in a positive way.
To increase your emotional resilience to negative or undesired emotions, think PLEASE.
Unmitigated stress can hurt your health
Our mind, body, and soul are all interconnected. How we treat our bodies has a major impact on our minds and our soul, and vice versa. It’s important to know how we are contributing to our emotional vulnerability. Life is hard. Emotions are raw and real. It’s important to understand how you may be contributing to your emotional vulnerability.
What is vulnerability?
Vulnerability is the quality or state of being exposed to the possibility of being attacked or harmed, either physically or emotionally. In other words, when we leave a vulnerability unattended, we are opening the door to being physically and emotionally harmed.
Often when we feel emotionally vulnerable, we are in a state of mind called “Emotion Mind”. Emotion Mind is when our emotions run rampant, we engage in mood-dependent behavior and our “emotions get the best of us.” Emotional distress can be reduced by decreasing factors that make us more vulnerable to negative emotions and moods.
To increase your emotional resilience to negative or undesired emotions, think PLEASE.
PL: Treat PhysicaL Illness- Being sick lowers your resistance to negative emotions. The healthier you are, the more likely you’ll be able to regulate your emotions. When you are injured, observe the urge to “just wait it out.” Often times we may think, “I should be able to power through this,” or “it’ll get better on it’s own.” See a doctor, chiropractor, dermatologist, or a specialist when needed. Reflect on what interferes with you attending to your physical illness and work toward problem solving the barriers.
E: Balanced Eating- Focus on eating balanced meals that make you feel good and avoid eating foods that upset your stomach or make you feel lethargic. Be mindful about urges to engage in emotional eating or eating out of boredom. Both eating too much and excessive dieting can increase your vulnerability to Emotion Mind. Research indicates that “self-imposed diets” show negative effects of eating too little. In other words, the more you restrict your food intake, the more likely you are to binge eat or having psychological problems (preoccupation with food/eating, increased emotionality and dysphoria, and distractibility). When you eat balanced and nutritional foods, you are less likely to have emotional control.
A: Avoid Mood Altering Substances: Alcohol and other substances, like certain foods, can lower resistance to negative emotions. Stay off illicit drugs and use alcohol in moderation. All substances, including caffeine and nicotine, increases our emotional vulnerability. Some of us may not feel an increase in emotional vulnerability while under the influence, rather experience Emotion Mind the days after.
S: Balanced Sleep: An increasing amount of research indicates that lack of sleep is related to a wide variety of emotional difficulties. Sleep is often undervalued in our culture. As a society, we are busy and constantly getting things done that we tend to slack on getting to bed at a decent hour. For people who work long hours, are single parents, are taking care of their loved ones, we tend to put sleep on the backburner. Maybe 11pm at night is the only “me” time you have, and you really want to catch up on the show. The thing about sleep is, we can’t “catch up” on it. There is no “making up for lost sleep.” Making sure you get the amount of sleep that feels right for you and your body is one of the most important variables to overall emotional well-being. Some people need 7 hours and other people know 10 hours. It’s also important to maintain a sleep routine, especially if you have difficulty sleeping. How much sleep do you need?
E: Get Exercise: Aerobic exercise, done consistently, is an antidepressant. Not only is exercise great for our our physical health, it’s great for our emotional well-being. Try and get some type of exercise every day. 20-30 minutes of cardio a day can increase emotional resilience. When your body is strong and healthy, you are less likely to slip into Emotion Mind and will feel less vulnerability overall. If you are new to exercising, build mastery. Start with 10 minutes and slowly increase the amount of time. Find a workout that is FUN that you WANT to get up and attend. You are more likely going to engage in physical activity if you are doing something that you look forward to. For some of us, that won’t be going to the gym for 1 hour. It may be running outdoors, spin class, yoga, dance classes, and other group classes (group classes are great for meeting people!)
Today’s guest blogger is Marissa Colangelo. Marissa Colangelo is a Licensed Clinical Social Worker (LCSW) with Compass Behavioral Health, specializing in treating adolescents and adults with emotion dysregulation, primarily personality disorders, anger, depression, impulsivity, substance abuse, and anxiety.
Putting Your House in Order: Food Reigns Supreme
Is eating gluten/lectins, grains and legumes problematic? Let’s focus on the elephant in the room: diet. It’s time for a gut check; by definition a gut check is an honest reflective appraisal of one’s true feelings regarding a matter of concern.
Wouldn’t it be nice if managing one’s health was like maintaining a clean home? Make the bed, empty the dishwasher, swiffer the floors, cleanse the sinks and tubs, tidy the countertops, use some floor mats and don't forget your annual window washing. Only green cleaners, right? Barring any catastrophic natural disasters, a two-minute shower while your four year-old is unsupervised, or an ant infestation (anyone else in OC relate to this?) the formula is rather simple.
On the other hand, obtaining a clean bill of health from your doctor can feel complex and downright overwhelming. Perhaps you are not feeling well, but your doctor(s) can’t seem to find anything wrong. You might be wondering if you have taken the right tests and had a thorough work-up. Conversely, maybe you are pre-diabetic, struggling with hypothyroid, joint pain, skin rashes, bouts of anxiety and depression, and migraines. You have been prescribed a host of medications and you’re expected to remain on those meds into perpetuity. You may be searching for a sustainable solution, one with fewer side effects, and one that allows your body to heal from the inside out. By and large, we underestimate the potential of food, sleep, and stress management.
Setting yourself up for a life free of disease and vigor in today’s society may feel like a pipe dream for a growing majority. I’d argue that there are a handful of reasons this is such a common dilemma.
Mismatch between diet and activity levels.
Change is hard, reinforced patterns are easy
The “attention economy” does not provide valuable education
Repetitive insults to the gut, immune system and metabolism go unchecked
A one size fits all healthcare approach
Conventional medicine is designed for disease management and not prevention
Most medical paradigms do not “aim at the origin” and/or discount the body’s interconnectedness
Lifestyle interventions are time-intensive and difficult to align with insurance- based care
Diagnostic testing is looking downstream
Poor diagnosis and treatment plans do not educate or empower the patient
Let’s focus on the elephant in the room: diet. It’s time for a gut check; by definition a gut check is an honest reflective appraisal of one’s true feelings regarding a matter of concern. How and what we eat is either optimizing our health or initiating new underlying pathology and eventually disease. For example, patients struggling with supporting thyroid function may need to address gut function to fully combat symptoms of hypothyroidism.
Risk factors for developing Digestive Pathology.
Chronic Stress
Sleep Deprivation
Physical inactivity
Hypothyroidism
HPA Axis dysfunction
Excess Alcohol
Environmental toxins.
Family History
Cesarean Birth
Formula fed
Standard American diet
Food poisoning
Antibiotics
Medications
The evolving role of diet has altered the way we understand disease. In fact, digestive health has a wide array of implications. Intuitively, this should not be a surprise. The gut is one of our main interfaces with our external environment, it houses trillions of bacteria, has its own nervous system and gut-associated lymphoid tissue (GALT).
The digestive system is both resilient and dynamic. This is a double-edged sword because it is really good at masking the effects of a poor diet. What happens in the gut is so powerful that it has long-distance effects on the brain, skin, skeleton, muscles, metabolism, cardiovascular system, endocrine system, and immune system. It’s not like the “what happens in Vegas stays in Vegas.” Take a look at figure 3. These examples of reactivity may be the result of something called molecular mimicry. Due to the similarity in molecular structure with food we eat and our own tissue, the immune system can be fooled into attacking look-a-like molecules that make up our own tissue leading to autoimmune disease.
Educational resource from Cyrex Laboratories.
Below is my own list of the top 10 effects of a poor diet:
6 Joint pains
7 Neurodegenerative syndromes
8 IBS and GERD
9 Dermatitis and eczema
10 Constipation
1 Diabetes
2 Obesity
3 Cardiovascular disease
4 Autoimmune disorders
5 Anxiety and Depression
So how do we detect, avoid these problems and remedy our diet. Some patients have symptoms like gas, bloating, constipation, abdominal pain and cramps, skin rashes, diarrheas, excess gas, brain fog, heartburn, excessive hunger, and other complaints. However, there are patients that do not have symptoms or have symptoms that seem unrelated. For example of those diagnosed with Celiac Disease, autoimmunity to gluten, only 50% have GI symptoms.
With advances in research we have a better understanding about gut pathologies such as intestinal permeability aka “leaky gut,” food intolerances (tend to be undiagnosed), celiac disease and non-celiac gluten sensitivity, hypochlorydia, gut dysbiosis, small intestinal bacterial overgrowth (SIBO) and infections.
A functional medicine approach is a great way for patients to understand what is at the root of their health challenges. What that looks like for most patients is an extensive history, some form of altered diet (in some case removing gluten, wheat and dairy) and tests or screens for:
Wheat/Gluten reactivity
gluten-associated cross-reactivity
pathogen screens
intestinal permeability
SIBO
and other tests depending on a working diagnosis.
Treatment protocols are designed for each patient and tend to employ a mixture of dietary restriction, antimicrobials, pro/prebiotics, and other temporary supplementation meant to heal the gut
Researchers and clinicians continue to unravel the different mechanisms behind health pathology. There is some controversy regarding food intolerances, dysbiosis, leaky gut, autoimmunity, and hormone dysfunction. However, novel screening tools and continued research help shed light on how to treat the source of the problem and return your overall health.
If you have questions please email them to nick@spineandjointoc.com