SATURATED FAT & CHOLESTEROL: THE HEART DISEASE SCAPE GOAT ( Part 3)
At the core of any diet there are two fundamental truths when it comes to eating for your health.
Number 1: Avoid processed and refined food
Number 2: Choose nutrient dense foods and incorporate healthy/traditional fats
What does PUMP mean?
Welcome Back! Continuing from part 2. Now we are going to build on the basic info and screening tools. We’ll touch on the more advanced markers to help stratify an individual’s risk for cardiovascular disease. Remember these tests are not bulletproof data points. It’s not a black and white process. A thorough history, review of systems and specific health assessment measures can provide a great blueprint.
Plates not Pills
Armed with that information patients may take the necessary dietary and lifestyle changes to improve how they feel, decrease negative symptoms and see blood markers normalize. You would be hard pressed to find doctors that would deny lifestyle modification as the primary form of intervention. It’s always a good idea to consult with your physician to discuss medication and track your overall heart health.
Useful markers/tests for determining cardiovascular risk
* Included in an Iron panel: serum iron, TIBC, UIBC iron saturation aka transferrin saturation
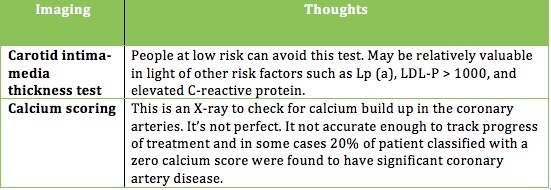
Two Additional tests that some physicians utilize.
Without a needle or Imaging
If you’re inclined you may want to use one of these two online calculators to give you a basic sense of your risk for heart disease.
If you are over twenty years of age and do not have heart disease or diabetes you can calculate your risk using the Framingham 10-year Risk Calculator. The inputs include: age, gender, total and HDL cholesterol, smoking status, and blood pressure. The Reynolds Risk score might be a better option. It includes family history and C-reactive protein.
If you are ready to minimize your risk, limit your medications and learn what makes up a heart-healthy action plan read on.
In the spirit of heart health
I’ve come up with a mnemonic to help you understand the right approach. PUMP
P - purposeful eating
U - understand your risk
M - measure to be sure
P – participation and lifestyle modification
Over the course of these 3 articles we’ve brushed up on the 3-legged stool of heart disease: (1) why it happens, (2) what causes it, and (3) what’s your risk. Let’s talk about the seat of the stool as it holds all of the legs together and acts as the cornerstone. In this analogy the seat can be divided into 3 parts: Diet, weight management, and exercise.
If you are overweight and want to reduce your risk of heart disease without the side effects of medication eating with purpose will help you lose the weight. Improving one’s relationship with food must be tailored to the individual.
At the core of any diet there are two fundamental truths when it comes to eating for your health.
Number 1: Avoid processed and refined food
Number 2: Choose nutrient dense foods and incorporate healthy/traditional fats
Why? Eating this way curbs inflammation, hunger, weight gain, and metabolic syndrome (recall 1/3 Americans are estimated to have MetS).
From a bird’s-eye view the majority of food should come in the form of meat, poultry, fish and shellfish, non-starchy vegetables, starchy tubers, fruit, nuts, and seeds. Sorry guys please don't try and find these items at Olive Garden or Taco bell.
If you are currently floundering on the standard American diet (SAD) this may feel a bit like an elimination diet. How many daily grams of carbs does the average American eat? Take a guess. It’s around 300 to 400 grams of carbs per day! Delicious, I know. However, the lion’s share comes from refined carbohydrates such as breads, cereals, chips, pasta and crackers. A more sensible target, utilizing whole foods, puts one at 50 - 250 grams of carbs per day. So you’re wondering — Is he suggesting that I go on a plant-based, keto, paleo, or an atkins-like diet? Can I drink milk and eat pizza and pasta?
I am suggesting some form of a modified paleo-ish diet. As for dairy it’s best to eliminate for one month and add it back in to see how it’s tolerated. Eliminating grains entirely may be a hard sell, but you won’t know how you feel or how you’re body will change if you don't give it shot. It doesn’t get much attention, but grains contain certain anti-nutrients that can cause digestive problems and other stealth health issues.
Let’s talk turkey (of the sea)
The average American eats a ratio of anywhere from 12:1 to 25:1 Omega 6 to omega 3 fatty acids. This creates a highly inflammatory state. Usher in some cold-water fish. Some studies suggest that eating 8 oz of fish / week (we’re not talking tilapia; it’s farmed and high in omega 6) would equate to 20,000 few deaths from CVD and 4,000 fewer nonfatal strokes. It’s been speculated that regular fish consumption may reduce total mortality at a higher rate then statins (statins garner 40 billion dollars a year and is a article in itself).
So if not tilapia? We want fish high in omega 3 such as salmon, mackerel, herring, sardines, anchovies, and bass, as well as shellfish like oysters and mussels. The single highest seafood source of EPA and DHA is caviar or fish eggs. I could not eat fish eggs if my life depended on, but if you like them more power to you.
If you want to hit a clinically relevant range of omega 3’s you want to eat 3.5 EPA plus DHA per week. This may reduce heart disease by as much as 25%. A good goal would be to eat between 10-16 oz of fatty fish/shellfish per week. Make up any short fall with a high quality fish oil supplement.
When it comes to other healthy fats olives, olive oil avocados, and macadamia nuts provide healthy monounsaturated fats. Remember monounsaturated fats have been shown to reduce LDL and Triglycerides, decrease oxidized LDL, lower blood pressure, decrease thrombosis, and reduce incidence of heart disease.
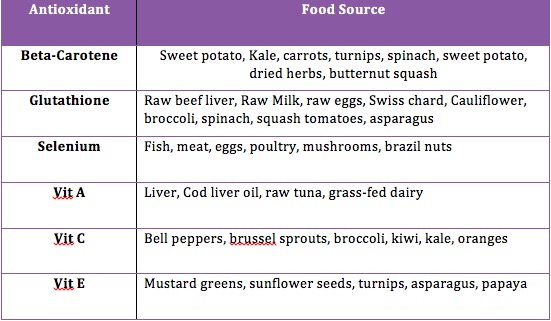
You might be familiar with the term antioxidants. If you recall shortages in antioxidants may contribute to an increase in oxidized LDL, which is associated with arterial plaque build up. Food companies do an excellent job with their packaging to seduce the consumer. The supplement and nutraceutical industry is vying for you to seek out their pills. While supplements may be beneficial in some situations, it’s preferable to get these nutrients we need from whole foods, Mother Nature, and not isolated synthetic sources like ascorbic acid.
There is mixed support in the medical literature on antioxidant supplementation. You may have heard that treatment with beta-carotene, vitamin A and vitamin E may increase mortality. For reasons we that have not been fully discovered whole foods appear to be more effective than supplements in meeting nutrient requirements.
Foods high in antioxidants (lower oxidative stress and inflammation) include leafy greens and berries, but there is more to the story. Red meat and organ meats are also rich in antioxidants that are not found in significant amounts in plant sources.
I don’t want to go any deeper into the nutritional weeds. Remember there is no one-size fits all approach. Ultimately, a heart healthy diet requires some attention. It starts by eliminating processed foods and switching to nutrient dense whole foods. There should be an emphasis on cold-water fatty fish and shellfish, healthy fats, antioxidants rich foods, polyphenol-rich foods, soluble fiber, nuts, fermented foods and occasional alcohol. If you decide to supplement be selective. For example, it’s better to take folate then the synthetic folic acid. Much of folic acid is never converted to folate.
Back to the stool analogy
Earlier I broke the stool seat into 3 parts, diet, weight management, and exercise. For most people combining diet and exercise will help you reclaim a healthy weight. The evidence is pretty straightforward and suggests that regular moderate exercise prevents the build up of arterial plaque, improves lipids and reduces vascular symptoms in people with heart disease. Exercise is a great way to reduce stress, and you may have heard me cite stats on the interplay of stress and risk of cardiovascular disease. I’m not proposing everyone flock to the nearest HIIT gym or LA fitness. Make small changes based on your current activity level and attempt to log 10,000 steps a day.
Questions
If you have any specific questions regarding this 3-part educational series (testing, supplementation, lowering high blood pressure, or statin drugs) please contact me at nick @spineandjointoc.com
SATURATED FAT & CHOLESTEROL: THE HEART DISEASE SCAPE GOAT (Part 2)
When analyzing one’s risk for heart disease some combination of looking at the big picture and using more micro-level blood markers will serve you well.
Now that we know a little more about cholesterol and saturated fat it’s time to refocus on the villains. What factors lead to an increase in LDP particle number and oxidized LDL?
An increase in LDL particle number has been directly associated with Metabolic syndrome (MetS). Research estimates that people with MetS are approximately 3x more likely to have an elevated LDL particle number.
So what is MetS? The criteria have changed over the years, but here is the general consensus.
ANY three of the 5 Criteria below:
Obesity -- Waist circumference >40 inches for male and >35 inches for females
Hyperglycemia -- Fasting glucose ≥ 100 mg/dl or pharmacologic treatment
Dyslipidemia – Trigylcerides ≥ 150 mg/dl or pharmacologic treatment
Dyslipidemia (separate criteria) – HDL cholesterol < 40md/dl male, < 50 mg/dl females; or pharmacologic treatment
Hypertension -- >130 mmHg systolic or > 85 diastolic or pharmacologic treatment.
*Note: LDL particle (LDL-P) number appears to be the most accurate marker for predicting metabolic syndrome. How do you test LDL-P. A test called NMR lipoprofile. More on this later.
For those that meet this criteria there are some common themes. Increased LDL particles (more triglycerides to shuttle around), leptin resistance, insulin resistance and excess body fat. If you have metabolic syndrome and insulin resistance your risk of heart disease is elevated even with subclinical levels of LDL cholesterol and total cholesterol.
In addition to MetS there are several other factors that may contribute to increased particle number. These include infections, poor thyroid function, and genetic mutations (familial hypercholesterolemia or ApoE4).
Similar to elevated LDL–P an increase in oxidized LDL has four primary causes.
1. LDL particle vulnerability (the type of fatty acids in the membrane may account for increase in LDL oxidation). Think omega-3 vs. omega-6 ratios
2. Antioxidant shortage (Eating processed foods without the right cofactors and enzymes)
3. High levels of oxidative stress (smoking, stress, lack of exercise, environmental toxins and infections)
4. Time (poor LDL clearance from the blood stream)
Here is where the rubber meets the road.
How to assess your risk of heart disease.
It doesn't hurt to take an honest look at your body composition, weight and physical fitness. Next a standard lipid panel. Never mind its inadequacies, it’s an okay starting point (see sample result.)
What is a normal cholesterol level?
There is some debate, but in the US the cutoff for total cholesterol is 199 mg/dl. Here is where some context comes into play. Studies looking at traditional populations around the world appear to tell a different story. When you look at the Massai tribe of east Africa, Inuit, Kitiva, the Tokelau, and Pukapuka we see cholesterol levels anywhere between 140 and 250 mg/dl. The kicker is they are all relatively free or completely free of heart disease.
Err on the side of caution
If some of your cholesterol levels are out of range further testing is recommended.
· Total cholesterol >299 mg/dl
· Cholesterol/HDL ratio > 4 or HDL < 40 mg/dl
· Triglycerides >125
Since total cholesterol and LDL cholesterol are not always reliable markers it’s best to avoid taking a statin based on a single standard lipid panel. This is especially true if you intend to make lifestyle changes such as increased exercise and dietary modifications.
Keep in mind that a single cholesterol test is of limited value. Why? Your total cholesterol can fluctuate by 35 mg/dl up or down. Triglycerides exhibit greater variability 40 up or down mg/dl. Let me be very clear that high quality large research studies indicate that LDL particle number, and not LDL cholesterol (measured on standard lipid panel), is the more significant risk factor.
One way to use the standard lipid panel and extrapolate risk would be to look at your Triglycerides (TG). If levels are below 125 mg/dl LDL particle number and LDL cholesterol coincide. However as that TG number climbs (>125) LDL particle number and LDL cholesterol diverge. The relationship stops and particle number rises.
Life after a standard lipid panel
If your numbers are outside of the medical ranges you may want to retest with an NMR lipoprofile. This test can be ordered through most blood labs (Quest, Lab Corp, and U.S. Healthworks). As with the standard panel there’s a lot of variation with LDL particle number so it’s important to consider retesting subsequent changes in diet and lifestyle. It important to note that your doctor may order a test for apolipoprotein B (ApoB). This is an indirect way to of measuring LDL particle number. ApoB is what forms LDL or low-density-lipoproteins.
If you’ve made it this far you’re probably wondering should I test for oxidized LDL. Based on what I’ve read Oxidized LDL is a strong risk factor for heart disease; however, measuring it directly is problematic, and it doesn’t appear to add any additional predictive value above and beyond LDL particle number. When analyzing one’s risk for heart disease some combination of looking at the big picture and using more micro-level blood markers will serve you well.
In part 3 we will talk about some other markers that may be relevant when understanding cardiovascular disease.
Disclaimer:
Please note that this information is not meant to provide medical advice or take the place of medical advice or treatment from your physician. I offer this for educational purposes.