Spanx and dad bods - what do they have in common?
If these terms are foreign to you. Spanx is a huge company that manufactures shape-wear to help men and women appear thinner. The term “Dad bod” (as defined by the Urban dictionary) is a male body type that is best described as "softly round."
The picture above is the Spanx warehouse circa 2019 (popped up on linkedIn and if I’m being honest served as the muse for this post)
If these terms are foreign to you. Spanx is a huge company that manufactures shapewear to help men and women appear thinner. The term “Dad bod” (as defined by the Urban dictionary) is a male body type that is best described as "softly round." It's built upon the theory that once a man has found a mate and fathered a child, he doesn't need to worry about maintaining a sculpted physique.
These products and this language are symptoms of large health issues.
If you are wondering, here are three common threads: a damaged liver, metabolism dysfunction and weight loss resistance.
If you have read some of my other posts then the term fatty liver syndrome is not all that new. When the liver is overburdened by excess sugar it will store fat, become insulin resistant and spark an inflammatory response.
Think about the combination of overly stressful lives and modern diets high in refined carbohydrates and excess calories. This is no walk in the park for the body. On the contrary, it's extremely taxing. If we are carrying excess weight over extended periods, the pancreas and the liver are taking a hit. Depending on how well your metabolism works people’s bodies respond across a broad spectrum.
Have you heard of the TCA cycle, also known as the Krebb’s or citric acid cycle? This cycle allows the body to burn food for energy by converting glucose into ATP. The more glucose burned, the less glucose in the bloodstream. Too much glucose in the bloodstream can have a damaging effect. It’s one reason why we check the biomarker hemoglobin A1C. It’s measuring the approximate damage to the red blood cells over the course of 90 days. Out of control glucose levels damage body proteins in the bloodstream, which in turn has damaging effects on the eyes, brain, kidney, etc. If high fructose is repeatedly making its way into your diet excessive fructose consumption can lead to excessive glycation of proteins (up to 16 times faster) than glucose.
Every day is a chance to right the ship a little bit at a time. The body is very dynamic and desperately prefers to be in an energy balanced state. Your DNA holds the blue print to a well functioning metabolism, but it needs a diet with the right type and amount of fuel.
If we can construct a daily routine that normalizes glucose, leptin, and insulin metabolism the benefits are Vast (with a capital V):
reduced risk of diabetes-related complications
(neuropathy, kidney or vision damage),
lower cardiovascular risk (lower blood pressure, triglycerides, increased HDL, better
endothelial function)
reduced cell proliferation (tumors), less water retention, less fat storage and easier fat release from the adipose cells.
In my experience when patients regain their metabolic flexibility they will see their blood pressure and high cholesterol normalize. And in the case of autoimmunity these markers improve as well. When I use the term metabolic flexibility I’m referring to humans ability to use, properly store, and breakdown different food sources.
Sayonara Spanx expenditures and dad stereotypes
When you are trying to repair your metabolism you need to layer in 4, possibly 5 things.
Better Sleep
Mitigate stress
Activity level
Food
Supplements in therapeutic doses.
Research shows that sleep deprivation can have profound metabolic and cardiovascular implications. Sleep deprivation, sleep disordered breathing, and circadian misalignment are believed to cause metabolic dysregulation through myriad pathways involving sympathetic overstimulation, hormonal imbalance, and subclinical inflammation (1). Some studies have shown that recurrent partial sleep restriction can create dysfunction of both glucose and lipid metabolism. Lastly, epidemiological data is suggestive of weight gain with sleep deprivation, although a few studies have also noted weight gain with prolonged sleep.
We know that perceived stress can have a similar impact as physical stress. Stress can be a thought or even the perception of a threat. If we loop back to stress and metabolism what we find is a cluster of disorders: Obesity, lipid disorders, type 2 diabetes, high blood pressure and coronary heart disease. When you are stressed your nervous system, specifically the sympathetic nervous system, activates a stress response. It does this through epinephrine and cortisol release. Over the long term these hormones decrease your body’s sensitivity to insulin. It hypothesized that cortisol may favor the development of central obesity. Hello flat tire and muffin tops.
Today we are faced with repeated professional or social stress and a small portion turn to exercise to help curb the stress and maintain weight. If your metabolism is broken it probably makes more sense to fix your nutrition, sleep and stress before you overhaul your workout routine. I’m not saying don’t exercise but it’s better to incrementally build up to more challenging training. As someone who works out 5-6 times per week, it's very important. If you are someone with the signs and symptoms of metabolic syndrome walking, occasional stretching (yoga) and micro workouts might be the better way to start.
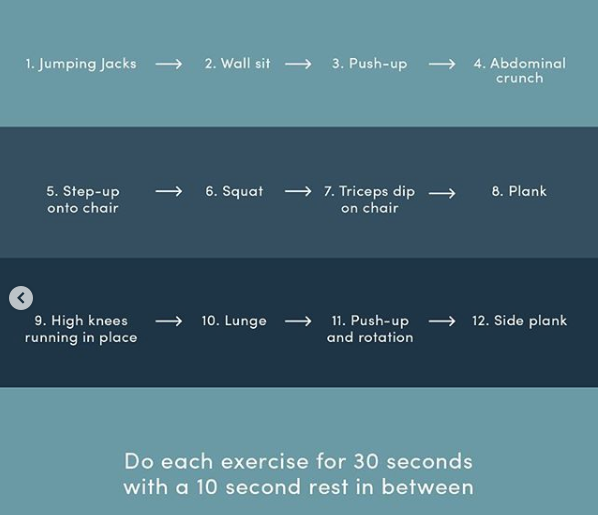
For example check out this quick circuit that Dr. Mark Hyman shared on social media.
This 7 minute workout has been shown to: decrease body fat, lower insulin resistance, and improve VO2 max and muscular fitness.
When you are struggling with weight loss resistance, diabetes, heart disease, or fatty liver, food can seem like an enigma. Let me be clear - sifting through all the information can be overwhelming and in some ways feel defeating. How you plan, package and execute will determine the degree of transformation. I’m going to avoid the gritty details and share a few patterns. If what to eat is the bane of your existence I would suggest two options. Start reading some of the new books on nutrition or work with a functional nutritionist until you feel you are ready for some autonomy. It’s never a bad idea to have functional medicine practitioner run a comprehensive blood panel to understand your baseline markers.
Let me preface these statements with:
Eat the standard American diet, get the standard American diseases.
No 1. When it comes to food “focus on taking the role of an impartial observer”. The food we eat is tied to our emotions and woven into our habits.
No. 2 Make sure you are eating to meet your energy needs.
No. 3 Say goodbye to bagels, cereal and flour (at least during the dietary intervention). Chances are you will be able to reincorporate down the line.
No. 4 Do not fall prey to overly restrictive fad “all or nothing” diets (there are exceptions). Give your body the vitamins nutrients and minerals by eating some meat and plants. Avoid foods with labels and if they have them read them!
The last I read the dietary supplements industry was at 122 billion a few years ago. It’s expected to grow another 100 billion. What can I say? We’re getting sicker and are open to magic pills. The reality is that some supplements have a place in nutritional care plans and therapeutic protocols. Once you find the right supplements they can be beneficial. For non-practitioners I’m not sure if it’s really possible to stay up to date on the best products. Moreover, understanding when and how to incorporate and test a supplements efficacy take some education. Along with diet and lifestyle changes supplements can be extremely powerful tools for treating and in many cases overcoming symptoms that present with metabolic disorders.
As always please email your health questions to nick@spineandjointoc.com
SATURATED FAT & CHOLESTEROL: THE HEART DISEASE SCAPE GOAT ( Part 3)
At the core of any diet there are two fundamental truths when it comes to eating for your health.
Number 1: Avoid processed and refined food
Number 2: Choose nutrient dense foods and incorporate healthy/traditional fats
What does PUMP mean?
Welcome Back! Continuing from part 2. Now we are going to build on the basic info and screening tools. We’ll touch on the more advanced markers to help stratify an individual’s risk for cardiovascular disease. Remember these tests are not bulletproof data points. It’s not a black and white process. A thorough history, review of systems and specific health assessment measures can provide a great blueprint.
Plates not Pills
Armed with that information patients may take the necessary dietary and lifestyle changes to improve how they feel, decrease negative symptoms and see blood markers normalize. You would be hard pressed to find doctors that would deny lifestyle modification as the primary form of intervention. It’s always a good idea to consult with your physician to discuss medication and track your overall heart health.
Useful markers/tests for determining cardiovascular risk
* Included in an Iron panel: serum iron, TIBC, UIBC iron saturation aka transferrin saturation
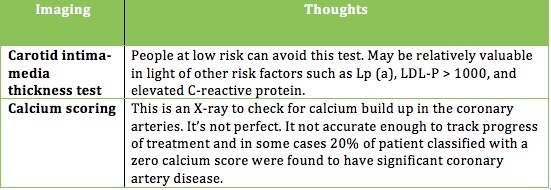
Two Additional tests that some physicians utilize.
Without a needle or Imaging
If you’re inclined you may want to use one of these two online calculators to give you a basic sense of your risk for heart disease.
If you are over twenty years of age and do not have heart disease or diabetes you can calculate your risk using the Framingham 10-year Risk Calculator. The inputs include: age, gender, total and HDL cholesterol, smoking status, and blood pressure. The Reynolds Risk score might be a better option. It includes family history and C-reactive protein.
If you are ready to minimize your risk, limit your medications and learn what makes up a heart-healthy action plan read on.
In the spirit of heart health
I’ve come up with a mnemonic to help you understand the right approach. PUMP
P - purposeful eating
U - understand your risk
M - measure to be sure
P – participation and lifestyle modification
Over the course of these 3 articles we’ve brushed up on the 3-legged stool of heart disease: (1) why it happens, (2) what causes it, and (3) what’s your risk. Let’s talk about the seat of the stool as it holds all of the legs together and acts as the cornerstone. In this analogy the seat can be divided into 3 parts: Diet, weight management, and exercise.
If you are overweight and want to reduce your risk of heart disease without the side effects of medication eating with purpose will help you lose the weight. Improving one’s relationship with food must be tailored to the individual.
At the core of any diet there are two fundamental truths when it comes to eating for your health.
Number 1: Avoid processed and refined food
Number 2: Choose nutrient dense foods and incorporate healthy/traditional fats
Why? Eating this way curbs inflammation, hunger, weight gain, and metabolic syndrome (recall 1/3 Americans are estimated to have MetS).
From a bird’s-eye view the majority of food should come in the form of meat, poultry, fish and shellfish, non-starchy vegetables, starchy tubers, fruit, nuts, and seeds. Sorry guys please don't try and find these items at Olive Garden or Taco bell.
If you are currently floundering on the standard American diet (SAD) this may feel a bit like an elimination diet. How many daily grams of carbs does the average American eat? Take a guess. It’s around 300 to 400 grams of carbs per day! Delicious, I know. However, the lion’s share comes from refined carbohydrates such as breads, cereals, chips, pasta and crackers. A more sensible target, utilizing whole foods, puts one at 50 - 250 grams of carbs per day. So you’re wondering — Is he suggesting that I go on a plant-based, keto, paleo, or an atkins-like diet? Can I drink milk and eat pizza and pasta?
I am suggesting some form of a modified paleo-ish diet. As for dairy it’s best to eliminate for one month and add it back in to see how it’s tolerated. Eliminating grains entirely may be a hard sell, but you won’t know how you feel or how you’re body will change if you don't give it shot. It doesn’t get much attention, but grains contain certain anti-nutrients that can cause digestive problems and other stealth health issues.
Let’s talk turkey (of the sea)
The average American eats a ratio of anywhere from 12:1 to 25:1 Omega 6 to omega 3 fatty acids. This creates a highly inflammatory state. Usher in some cold-water fish. Some studies suggest that eating 8 oz of fish / week (we’re not talking tilapia; it’s farmed and high in omega 6) would equate to 20,000 few deaths from CVD and 4,000 fewer nonfatal strokes. It’s been speculated that regular fish consumption may reduce total mortality at a higher rate then statins (statins garner 40 billion dollars a year and is a article in itself).
So if not tilapia? We want fish high in omega 3 such as salmon, mackerel, herring, sardines, anchovies, and bass, as well as shellfish like oysters and mussels. The single highest seafood source of EPA and DHA is caviar or fish eggs. I could not eat fish eggs if my life depended on, but if you like them more power to you.
If you want to hit a clinically relevant range of omega 3’s you want to eat 3.5 EPA plus DHA per week. This may reduce heart disease by as much as 25%. A good goal would be to eat between 10-16 oz of fatty fish/shellfish per week. Make up any short fall with a high quality fish oil supplement.
When it comes to other healthy fats olives, olive oil avocados, and macadamia nuts provide healthy monounsaturated fats. Remember monounsaturated fats have been shown to reduce LDL and Triglycerides, decrease oxidized LDL, lower blood pressure, decrease thrombosis, and reduce incidence of heart disease.
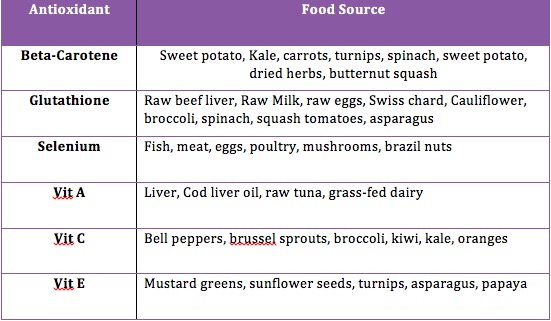
You might be familiar with the term antioxidants. If you recall shortages in antioxidants may contribute to an increase in oxidized LDL, which is associated with arterial plaque build up. Food companies do an excellent job with their packaging to seduce the consumer. The supplement and nutraceutical industry is vying for you to seek out their pills. While supplements may be beneficial in some situations, it’s preferable to get these nutrients we need from whole foods, Mother Nature, and not isolated synthetic sources like ascorbic acid.
There is mixed support in the medical literature on antioxidant supplementation. You may have heard that treatment with beta-carotene, vitamin A and vitamin E may increase mortality. For reasons we that have not been fully discovered whole foods appear to be more effective than supplements in meeting nutrient requirements.
Foods high in antioxidants (lower oxidative stress and inflammation) include leafy greens and berries, but there is more to the story. Red meat and organ meats are also rich in antioxidants that are not found in significant amounts in plant sources.
I don’t want to go any deeper into the nutritional weeds. Remember there is no one-size fits all approach. Ultimately, a heart healthy diet requires some attention. It starts by eliminating processed foods and switching to nutrient dense whole foods. There should be an emphasis on cold-water fatty fish and shellfish, healthy fats, antioxidants rich foods, polyphenol-rich foods, soluble fiber, nuts, fermented foods and occasional alcohol. If you decide to supplement be selective. For example, it’s better to take folate then the synthetic folic acid. Much of folic acid is never converted to folate.
Back to the stool analogy
Earlier I broke the stool seat into 3 parts, diet, weight management, and exercise. For most people combining diet and exercise will help you reclaim a healthy weight. The evidence is pretty straightforward and suggests that regular moderate exercise prevents the build up of arterial plaque, improves lipids and reduces vascular symptoms in people with heart disease. Exercise is a great way to reduce stress, and you may have heard me cite stats on the interplay of stress and risk of cardiovascular disease. I’m not proposing everyone flock to the nearest HIIT gym or LA fitness. Make small changes based on your current activity level and attempt to log 10,000 steps a day.
Questions
If you have any specific questions regarding this 3-part educational series (testing, supplementation, lowering high blood pressure, or statin drugs) please contact me at nick @spineandjointoc.com
SATURATED FAT & CHOLESTEROL: THE HEART DISEASE SCAPE GOAT (Part 2)
When analyzing one’s risk for heart disease some combination of looking at the big picture and using more micro-level blood markers will serve you well.
Now that we know a little more about cholesterol and saturated fat it’s time to refocus on the villains. What factors lead to an increase in LDP particle number and oxidized LDL?
An increase in LDL particle number has been directly associated with Metabolic syndrome (MetS). Research estimates that people with MetS are approximately 3x more likely to have an elevated LDL particle number.
So what is MetS? The criteria have changed over the years, but here is the general consensus.
ANY three of the 5 Criteria below:
Obesity -- Waist circumference >40 inches for male and >35 inches for females
Hyperglycemia -- Fasting glucose ≥ 100 mg/dl or pharmacologic treatment
Dyslipidemia – Trigylcerides ≥ 150 mg/dl or pharmacologic treatment
Dyslipidemia (separate criteria) – HDL cholesterol < 40md/dl male, < 50 mg/dl females; or pharmacologic treatment
Hypertension -- >130 mmHg systolic or > 85 diastolic or pharmacologic treatment.
*Note: LDL particle (LDL-P) number appears to be the most accurate marker for predicting metabolic syndrome. How do you test LDL-P. A test called NMR lipoprofile. More on this later.
For those that meet this criteria there are some common themes. Increased LDL particles (more triglycerides to shuttle around), leptin resistance, insulin resistance and excess body fat. If you have metabolic syndrome and insulin resistance your risk of heart disease is elevated even with subclinical levels of LDL cholesterol and total cholesterol.
In addition to MetS there are several other factors that may contribute to increased particle number. These include infections, poor thyroid function, and genetic mutations (familial hypercholesterolemia or ApoE4).
Similar to elevated LDL–P an increase in oxidized LDL has four primary causes.
1. LDL particle vulnerability (the type of fatty acids in the membrane may account for increase in LDL oxidation). Think omega-3 vs. omega-6 ratios
2. Antioxidant shortage (Eating processed foods without the right cofactors and enzymes)
3. High levels of oxidative stress (smoking, stress, lack of exercise, environmental toxins and infections)
4. Time (poor LDL clearance from the blood stream)
Here is where the rubber meets the road.
How to assess your risk of heart disease.
It doesn't hurt to take an honest look at your body composition, weight and physical fitness. Next a standard lipid panel. Never mind its inadequacies, it’s an okay starting point (see sample result.)
What is a normal cholesterol level?
There is some debate, but in the US the cutoff for total cholesterol is 199 mg/dl. Here is where some context comes into play. Studies looking at traditional populations around the world appear to tell a different story. When you look at the Massai tribe of east Africa, Inuit, Kitiva, the Tokelau, and Pukapuka we see cholesterol levels anywhere between 140 and 250 mg/dl. The kicker is they are all relatively free or completely free of heart disease.
Err on the side of caution
If some of your cholesterol levels are out of range further testing is recommended.
· Total cholesterol >299 mg/dl
· Cholesterol/HDL ratio > 4 or HDL < 40 mg/dl
· Triglycerides >125
Since total cholesterol and LDL cholesterol are not always reliable markers it’s best to avoid taking a statin based on a single standard lipid panel. This is especially true if you intend to make lifestyle changes such as increased exercise and dietary modifications.
Keep in mind that a single cholesterol test is of limited value. Why? Your total cholesterol can fluctuate by 35 mg/dl up or down. Triglycerides exhibit greater variability 40 up or down mg/dl. Let me be very clear that high quality large research studies indicate that LDL particle number, and not LDL cholesterol (measured on standard lipid panel), is the more significant risk factor.
One way to use the standard lipid panel and extrapolate risk would be to look at your Triglycerides (TG). If levels are below 125 mg/dl LDL particle number and LDL cholesterol coincide. However as that TG number climbs (>125) LDL particle number and LDL cholesterol diverge. The relationship stops and particle number rises.
Life after a standard lipid panel
If your numbers are outside of the medical ranges you may want to retest with an NMR lipoprofile. This test can be ordered through most blood labs (Quest, Lab Corp, and U.S. Healthworks). As with the standard panel there’s a lot of variation with LDL particle number so it’s important to consider retesting subsequent changes in diet and lifestyle. It important to note that your doctor may order a test for apolipoprotein B (ApoB). This is an indirect way to of measuring LDL particle number. ApoB is what forms LDL or low-density-lipoproteins.
If you’ve made it this far you’re probably wondering should I test for oxidized LDL. Based on what I’ve read Oxidized LDL is a strong risk factor for heart disease; however, measuring it directly is problematic, and it doesn’t appear to add any additional predictive value above and beyond LDL particle number. When analyzing one’s risk for heart disease some combination of looking at the big picture and using more micro-level blood markers will serve you well.
In part 3 we will talk about some other markers that may be relevant when understanding cardiovascular disease.
Disclaimer:
Please note that this information is not meant to provide medical advice or take the place of medical advice or treatment from your physician. I offer this for educational purposes.