Where to look if your health is stuck
It’s not unusual for one’s perspective on their personal health to change at different points in his or her life. For some there is indifference, frustration, and reactivity. For others there is clarity, deep involvement, proactivity, and even identity.
Each person has their own “health documentary.” Typically it’s a blend of factors that include your health history, family’s eating habits, psychological health, environmental factors, financial pressures, value systems, and other lifestyle habits.
I want you to pause and think about how you engage with your own health and possibly your family’s health. Do you think about the future of your health? Is it your responsibility or is it a transaction to be had with a doctor at a perfunctory check up? Are you competent enough to embrace your own inner doctor barring some critical situations?
You may be familiar with the term functional medicine. Functional medicine was born out of necessity. It is a systems-based approach that looks to reverse disease by identifying the drivers and causes. This form of personalized medicine is practiced by M.D.’s, D.C’s, D.O’s, Naturopathic doctors and a host of adjunct practitioners. Allopathic or conventional healthcare accels in acute situations and provides disease management. Where it is lacking is disease prevention and health optimization. If you only treat symptoms, people want pills. Show people the root cause and they will demand a fix.
For the most part you do not catch disease. You build it through life exposure, sometimes referred to as the exposome. The exposome is a collection of environmental factors, such as stress and diet, to which an individual is exposed and which can have an effect on health.
Let’s get back to your health. Imagine that you just landed in your body. Time for an appraisal. Can you move well? How do you feel? What’s your emotional and mental state? Is it a fixer-upper or does it require just some basic maintenance?
Perhaps you want to take a closer look at your physiology and chemistry by running predictive lab work. But before you even seek out a doctor, what is in your immediate control? Your lifestyle choices! Let’s touch on a few.
I. Manage stress wisely
Stress is a ubiquitous part of life that affects us all. Stress can have a profound effect on your gut. There is ample evidence that many chronic metabolic diseases start in the gut. Exposure to prolonged stress alters brain-gut interactions, ultimately leading to the development of a broad array of psychological and GI disorders.
II. Focus on nutrition
Food is one of the most effective tools for bringing balance to your body. When we optimize our diets we see improvements in detoxification, energy and metabolic health. We are a society in a chronically fed state. Too much processed foods derail our metabolism. Eating low-carb and the occasional keto cycle can retrain your metabolism and provide a necessary reboot.
III. Intermittent fasting
Our high school biology teachers failed to mention that fasting is not only a evolutionary skill , but also the best way to activate your body’s own “house cleaning” systems. It’s referred to as autophagy and it promotes healthy cell cycles and deep cellular detoxification. When paired with a proper diet it can help balance blood sugar, prune the microbiome, and build metabolic flexibility. Metabolic flexibility means your body can use protein, fats and carbohydrates efficiently.
VI. Exercise
Physical activity has endless possibilities. Research shows that we get the best results when we mix up our routines and change how we stress our bodies.
Fasted- cardio in the morning can help support healthy blood sugar and utilize body fat for fuel. (2-3 times per week)
Post-meal activity can put circulating blood sugar to work. This is 20-40 minute walks a few times a week after lunch or dinner.
High intensity interval training (HIIT) is a great way to work your metabolic machinery and increase insulin sensitivity (2 hours per week total)
Strength training you can’t go wrong having a higher proportion of muscle to fat mass ratio. Free weights, body weight, resistance bands all work well. (3 X per week 20-30 mins)
This article does not provide medical advice. It is intended for informational purposes only. It is not a substitute for professional medical advice, diagnosis or treatment.
Behavior Change - Rocket Powered Healing
It’s time to move away from the old “ diagnose and adiós” mentality.
Providing information alone or education is not a good recipe to change a behavioral or a pattern. Changing a person’s mind with information is tough whereas changing someone’s behavior with information is a true test.
We live in a fast-paced demanding world. It’s not unusual for us to create habits and even routines that help with the decision fatigue and a constant barrage of responsibilities. Some of these habits are by design and others just a default pattern. In some ways we are in “self preservation” mode.
Let me ask you – How many minutes per year do you spend on “habit change,” or “decision making.” It’s not really something we ponder, but maybe we should. Why? I’d argue that if we don’t we are more likely to go on cruise control and allow subconscious programming to guide our current behaviors. That inner pilot light that’s helping us close the gap on our goals, assess our progress, and change our behaviors grows silent.
So what do we have to do to enhance that inner voice and position ourselves to choose better behaviors? Dan Ariely, is a psychologist that uses a rocket analogy. It’s simple yet profound. Dan’s point is that we must change our environment in a way that reduces friction to make a desired behavior more attainable. Just as a rocket is designed with aerodynamics in mind people can minimize different types of resistance. Once friction has been reduced the rocket needs as much fuel as possible. Fuel in behavioral change is the motivation/energy or incentivizing factors.
How do we apply this analogy to actually making better choices. Providing information alone or education is not a good recipe to change a behavioral or a pattern. Changing a person’s mind with information is tough whereas changing someone’s behavior with information is a true test.
Instead we need to take it a step further and reduce friction by changing our internal environment and external environment. If that's true we already have a leg up on the rocket because we have more control over our external environment. Last I checked gravity does not fluctuate therefore it's a constant variable for the rocket scientists to overcome.
However, we have control over the people we choose to be with, the food that we eat, the relationships we foster, our attitudes, the dreams we pursue, and how we respond to our circumstances. And because our behaviors are often irrational it’s imperative we attempt to harness health related irrationality.
Similar to the mind our physical body responds to friction and fuel (here fuel is food, sleep, stress, social determinants, and mental attitudes).
Let’s look at 3 conditions people struggle with and then engineer ways to reduce the friction and fuel a sustained change.
LEAKY GUT
What creates friction?
Processed foods
Industrial seed oils
Multiple courses of antibiotics
Extended use of Antacids, histamine blockers and PPI’s
Unknown food intolerances
Bacterial overgrowth
Overtraining
Lack of sleep
How to reduce friction?
Create weekly meal plans
Allocate time to create a recipe list
Limit eating out
Test your gut
Look to natural remedies
Try an elimination diet
Intermittent fasting
Utilize a prebiotics and probiotic
Fatty Liver
What creates friction?
Overeating Leaky gut
Food intolerance
Poor bile production
Poor food choice
Endotoxins from GI tract
Alcohol in excess
Nutrient deficiencies
High blood sugar Medications
Bad Oils (seeds oils)
How to reduce friction?
Portion control
Eat for gut health
Liver support
Eat protein fats and some carbs
Liver blood work
Use time-restricted eating Intermittent fasting
Check thyroid health
Blood sugar and cholesterol problems
What creates friction?
Processed food consumption
Calorie surplus and high carb diet
Excess body weight
Insulin resistance
Elevated inflammatory markers
Genetic predisposition
Lack of activity
Emotional eating
Nutrient deficiencies
How to reduce friction?
Increase insulin sensitivity
Liver support
Eat protein fats and some carbs (Nutritional balance)
Use time-restricted eating
Check blood glucose with a glucometer after food (1hr & 2hr)
Check thyroid health
Get adequate sleep
What fuels these examples of friction?
Eating out (especially fast food)
Lack basic cooking skills
Poor time management
Not enough social connection
Poor sleep hygiene
Inability to cope with stress
Inadequate amount of downtime
Fuel to minimize friction?
An unhealthy gut creates problems elsewhere in the body
Gut problems may weaken your immune tolerance (autoimmune)
Gut problems may shift hormonal balance (i.e. PCOS, Cancer)
A dysfunctional gut suppresses our detox pathways
Leaky gut may interfere with your metabolism
What fuels these example of friction?
Disconnection from food choice and disease
Hyper-palatable foods (i.e. potato chips, pizza)
Ignoring constipation
Alcohol addiction
Not enough social connection
Lack of plants and animal products
Pill for every ill mentality
Oblivious to your lipid levels
Fuel to minimize friction?
We tend underestimate our dietary calories
Comprised liver leads to inflammation in the joints as well as the brain
Inflammation is linked to poor liver function
Liver health is directly connected to disease risk
A dysfunctional liver impairs our detox pathways
Liver can be compromised by 90% without a warning signs
What fuels these examples of friction?
Hyper-palatable foods (i.e. potato chips, pizza)
Giving in to cravings
Disregarding weight gain
Sugary drinks
Excessive snacking
Limited information from your doctor
Relying on basic lipid panels and subpar labs from a annual physical
Fuel to minimize friction?
Diseases associated with insulin resistance includes obesity, cardiovascular disease, nonalcoholic fatty liver disease, metabolic syndrome, and polycystic ovary syndrome(PCOS)
Gradual increase of physical activity and energy expenditure
Liver can be compromised by 90% without a warning signs
A dysfunctional liver impairs our detox pathways.
Sleep is necessary appropriate metabolic function
You may have noticed some of the overlap and redundancies, but that’s because there is an interplay going on in all these conditions. What’s going on in the gut directly affects the liver and both organs affect the cardiovascular system all the way down to each individual cell.
Leaky gut, fatty liver and blood sugar/cholesterol problems put a tremendous burden on the healthcare system and can subtract years of good health from just about anyone. Don’t fret because lifestyle modification should be the primary focus for treating any of these conditions.
The body is interconnected, complex, but also self healing. For example the The Diabetes Prevention Program and its Outcomes Study (DPP & DPPOS) demonstrated A 7% weight loss reduced the onset of type 2 diabetes (T2DM) by 58%. The best treatment for non-alcoholic fatty liver is weight reduction and correcting leaky gut and restoring immune tolerance can be done through shifts in diet, diagnostic testing, and targeted supplement protocols.
Given the importance of patient participation in healthcare decisions you deserve sufficient time and treatment solutions that require some self-management other than guzzling down a pill. It’s time to move away from the old “ diagnose and adiós” mentality. Never underestimate the changes you can make by learning about your health and assessing your habits. This exciting shift puts you in the driver’s seat of your life.
I’ll leave you with this, we don’t always do what’s in our own best long-term interest. With that in mind what will you do differently? Can you identify areas of friction and find your source of fuel?
Emptying the Dishwasher. Exposing a Lost Art.
So where does emptying the dishwasher come in? I have caught myself thinking about this a handful of times while emptying my own dishwasher.
When, how often and how we move has a profound impact on our health. The frequency and duration of movement affects our metabolism and how much fat we burn. It’s literally silencing hundreds of genes and activating others. Motion through the spine in tandem with a healthy cardiovascular system ensures that cerebral spinal fluid (CSF) moves through the ventricles in your brain and supplies the spinal cord with nutrients while removing waste.
Motion promotes joint and muscle health, which in return may keep pain at bay. Moving activates stabilizer muscles and helps balance overall muscle tone. Paying attention to our body mechanics promotes brain plasticity and strengthens new movement/motor circuits.
Movement can be used to help us regulate emotional states. It can help us regulate the autonomic nervous system (flight or flight vs rest and digest). The large majority of Americans are bombarded with stress and experience a hyperactive sympathetic response - exercise and motion is a great way to put the adrenaline and cortisol to good use.
So where does emptying the dishwasher come in? I have caught myself thinking about this a handful of times while emptying my own dishwasher. I’ve experienced that my own conditioned movements inadvertently put me in a less than ideal posture. We create “default neural networks” which means that the brain gets good at using certain pathways. This is especially true with our movement patterns.
A task as mundane as emptying the dishwasher seems like it would serve very little value. However, like most of our daily movements they have become automatic or predetermined if you will. Whenever we move we are either “ gaining ground or loosing it.” In other words, we are training healthy engaged movement patterns or causing harm.
I’ll be the first to admit that unloading the dishwasher is not Thai Chi or yoga for matter. These forms of exercise require precise “conscious movement.” However, I would encourage you to take a more mindful approach next time you fill or empty the dishwasher. Go through the whole process with awareness. This way you will witness how the whole body works together while gaining a better sense of structure and posture. From start to finish you will bend, flex, reach, push, pull, lift, rotate, look up, look down and hopefully get a few breaths in.
Think about a few things:
Are you bending your knees and hinging at the hips or straining your low back?
Is your weight evenly distributed or do you dump weight into one leg and or even a specific spot on the sole of your foot?
Are your upper trap muscles and neck tight with your head jutting out over your chest?
Is your upper body squared off or are you cockeyed?
When you reach to put away dishes is your core limp or activated. Does your arm elevate or does your whole shoulder move with it?
Are you tuned in to what muscles are activated? Do you know what your posture looks like as you transition between sorting the cutlery and sliding the racks back into place?
Are you moving in a conscious matter or allowing for poor body mechanics due to muscle imbalances, prolonged static postural stress, lack of movement variety and overall sedentary lifestyle.
Are you familiar with the statement “where the mind goes the body follows?” This simple concept of body awareness and our power to create and change is an active process. Today it’s not part of our normal routine to set aside some energy to restore healthy movement patterns. At any moment we are presented with an opportunity to cultivate more engagement and check-in with how we move.
A little bit of extra effort and examination on how we move may be the very thing that negates the need to pop some ibuprofen, saves you a trip to your ortho, keeps you in the gym, or even allows you to hold your grandchild without aches and pains. I’d gently implore you to pay a little more attention.
“Broken & Unaccountable:” American Healthcare – What to do instead?
As a chiropractor using functional medicine I have seen first hand that appropriate care is not being delivered for the root cause of illness. Drugs and surgeries are prescribed in way that forestalls the inevitable continuation of underlying pathology.
Many health professionals, especially early in their careers, would tell you healthcare is a calling. I’m not sure that there is a better job in the world than taking care of a patient. There are many doctors that are trying to fix the problems, but are facing some very strong headwinds. We’ve inherited a system that makes it difficult to prioritize the patient without neglecting the business’s bottom line.
As a chiropractor using functional medicine I have seen first hand that appropriate care is not being delivered to treat the root cause of illness. Drugs and surgeries are prescribed in way that forestalls the resolution of underlying pathology. If you have high blood pressure does it make sense to artificially lower it, or treat the cause of elevated blood pressure.
We all deserve healthcare that is patient-endorsed and that gets results.
What is driving healthcare problems?
Consumers have waited for politicians to ride to the rescue
There is a cost crisis and total lack of price transparency
Preventative care is rarely covered
Delivery of care is not designed to treat the root cause
Medicine is overprescribed (in 1997 2.4 billion prescriptions were written. By 2016 that number doubled to 4.5 billion)
We’ve all been taught that if you are going to criticize something that you should supply an alternate solution. Numbers 1 and 2 open up Pandora’s box. Therefore I’ll share a few observations and opinions, but spend the majority of this article on numbers 3,4, and 5. I’ll provide a case study that should help the reader relate to how this applies to you.
The media and politicians have polarized public opinions on healthcare and will continue to perpetuate this two-sided affair. You’re either pro affordable care act (ACA) or anti-ACA. You support a one-payer system or you believe in free market and competition. In reality it’s much more involved and we have yet to establish a meritocratic approach that reins in the cost, optimizes the delivery of valuable care, and ensures all Americans access to care.
This is especially important when speaking broadly about chronic disease (diabetes, obesity, heart disease, hypertension, fatty liver disease, etc) because it’s responsible for approximately 80 % of healthcare expenditures in the US ($3.5 trillion in 2017)
Did the affordable care act accomplish some things? Not denying people insurance with pre-existing conditions and keeping kids on their parent’s plans until 26 is embraced by the large majority. Did the ACA lower the price of health insurance in the United States by $2,500 per year? No! Will getting rid of it fix healthcare? I would argue that it would not, because in order for healthcare to be fixed we need a total re-haul. Does conventional medicine excel at preventing or reversing chronic disease?
The US healthcare system runs on a fee-for-service model where doctors get paid for the pills and surgeries they prescribe. This rewards quantity over quality. Doctors don’t get reimbursed for spending time with patients counseling them on the benefits of healthy eating and other lifestyle modifications. Until that reimbursement model changes medical care and education will continue on unchanged.
We need to be aware of what’s happening in the medical system.
A national study found that 21% of medical care was deemed unnecessary by physicians
A new study out of John Hopkins details how 48% of all Federal spending goes to healthcare
1 in 5 Americans have medical debt in collections
There is zero transparency when it comes to healthcare costs. Predatory billing and price gouging are hard to detect, but are commonplace.
The current system plays a game of inflating prices for insurance companies and making exorbitant amounts of money on the backs of patients. The days of plans with great benefits are gone.
Outside of your monthly premium it’s nearly impossible to know how much you will pay out of pocket, what the hospital or doctor will bill the insurance, and the degree to which what you paid for was medically appropriate.
People are getting crushed by their premiums and our health continues to deteriorate. If you’re interested in learning more about cost crisis and how to navigate within conventional medicine see the link Dr. Marty Makary new book, The Price We Pay.
Most doctors want to provide meaningful care to their patients.
What this means to me is keeping patients out of disease and empowering them to take health into their own hands.
If we look at the statistics around chronic disease it demonstrates that the current approach to healthcare is failing. Until patients have the right platform we will continue to go in the wrong direction.
Why don’t expensive insurance plans pay for the tests and therapy we need to prevent and fix disease at its core?
In the 1960’s the AMA [American Medical Association] agreed to drop its opposition to Medicare and Medicaid. They demanded that the new laws would back usual, customary and reasonable fees.
This was the beginning of ‘corporatized” care that lead to disproportionate fees for hospital visits, surgery, and technologic procedures for treating acute illness. Where reimbursement waned -- office visits for maintenance, treatment of chronic illnesses and/or for prevention. It’s important to note that during the time these fee structures were developed much of what we know about preventative evidence-based care has changed dramatically.
When creating a treatment plan or in doctor speak an “interventional therapy”, you should aim for a plan with a “curative effect.” Sounds simple but conventional medicine is not designed to provide us a cure. It’s meant as a way to manage disease.
Here is a very simple example. Patient goes to primary care doctor. Blood tests are run and results show high LDL cholesterol and triglycerides. Doctor then prescribes a statin drug to decrease cholesterol production and runs a basic lipid panel every year for 20-30 years while re-filling the prescription.
You should know that statins have not been shown to extend the lifespan in men under the age of 80 without heart disease, in women of any age, and in men over the age of 80 with heart disease. Moreover, statin side effects are often underreported!
If you have read any of my articles on heart disease you know that what’s important are the LDL particle numbers (lipoproteins) as well as markers for diabetes and inflammation.
How should you approach medical care?
Start with P4 medicine.
Personalized
Predictive
Preventative
Participatory
Healthcare practitioners want to spend our time on things that matter. So what matters to the patient?
Getting answers
Piece of mind
Understanding the treatment
The total perceived value of the care
Personalized care
Getting them back to what’s important in their life
Being included in the decision making process
Integrated care based on patient priorities
At this point in time if you are looking to stay healthy, reverse chronic disease, or even obtain a diagnosis you will have to do some work. This might mean working with an integrated team. For example I assist patients that are working with an endocrinologist, an obstetrician, personal trainer, and a psychiatrist. It’s key to find providers that can spend enough time with you. You will have to pay more up-front, but you will save beyond your wildest imagination long term.
Case Study: Functional medicine approach
Let’s talk about Karen. She is a 41-year-old, 5’4” woman who weighs 165 pounds and is premenopausal. Her goal weight is 135 lbs which was her weight before becoming pregnant with her second child.
She goes to the gym 3 times per week and performs some type of cardio i.e. elliptical or gentle yoga. She drinks red wine a few nights a week and has a self-confessed sweet tooth. She was recently diagnosed as pre-diabetic. Five years ago she was diagnosed with thyroiditis, but was told last year that her thyroid is “okay.”
She doesn’t sleep well and stays up late watching tv sometimes. She suffers from bloating and stomach upset. Conventional doctors have been unable to diagnose her with any gastrointestinal issues. She has tried Weight Watchers and paleo, but regains whatever weight she loses. Based on her 24-hour food diary her total calorie intake is about 2,400.
What are some of the things we did?
Recommend a “simple” Paleo diet template that provides around 1,900 calories per day, 25 percent protein (about 110 g), 25 percent carbs (about 110 g), and 50 percent fat (100 g). What the heck does that look like?
10 to 12 ounces of meat/chicken/fish/eggs
1.5 to two cups of starchy plants
one serving fruit
six tablespoons of added fats
We gave the patient the option of intermittent fasting with an eight-to-10-hour feeding window and suggested that she consume the recommended amount of food within that window.
We recommended that the patient get the following testing: SIBO breath test, Cyrex testing (as finances allow), and stool testing if needed. In her case we performed the stool test as her TSH levels were elevated as were her Anti-TPOs and it’s important to see if microbial imbalances may be promoting autoimmunity.
We ran a cardiometabolic panel and a full thyroid panel.
After 3 months of treatment (targeted supplementation, dietary and lifestyle modifications) Karen was able to loose 20 lbs. Her SIBO retest came back negative, and her blood sugar improved (HgA1C, fasting blood glucose and insulin). She has had 1 or 2 episodes of bloating, but her stomach pain has resolved.
What these results mean
Karen feels like she has control over her diet and weight
She won’t need to be on insulin or metformin in the future
She’s decreased her cardiovascular risk profile
She won’t need to take thyroid medication (at least not in the near future)
She has improved energy and anxiety has decreased since her stomach pain resolved.
This was a bit longer than I intended so I’ll wrap it up.
The best part about taking a comprehensive approach is the opportunity to “upgrade” a patient’s overall paradigm of health to one of prevention and empowerment as opposed to passive and reactive therapies.
Keep advocating for your health. Map ouT your health risk(s) sooner than later .Try to find resolution to health concerns now so that you can avoid the future pills, surgeries, and medical bills.
Is your metabolism sick: 9 ways you may be hurting your metabolism
The average woman in the US today weighs 168 pounds. This is approximately the same as an average man in the 1960’s (CDC). Men are up 30 pounds and 20% of children are obese.
1.Weight
Let’s start with the low hanging fruit. Research in the 90’s determined that the overwhelming majority of women— 89%—want to lose weight and 3% wanted to gain weight. In contrast, 22% of the men who were dissatisfied with their weight wanted to gain weight. Today Americans are eating more calories than we ever did in the past. More importantly refined sugars and flour make up the larger part of the pie when compared to whole foods i.e. vegetables, fruits, meat, poultry, seafood.
The average woman in the US today weighs 168 pounds. This is approximately the same as an average man in the 1960’s (CDC). Men are up 30 pounds and 20% of children are obese.
As a nation we are addicted to convenient, hyper-palatable large portioned options and it is taking its toll in more ways than one. The prevalence of non-alcoholic fatty liver, diabetes, obesity and cancer move in lockstep with a dysfunctional metabolism. It would be an understatement to say Americans are confused about food choices. Most are perplexed and making personal choices that provide the knockout punch to a struggling metabolism.
2.Overeating
Yes, food choice matters! Deciding to have repeat bagels or cereal instead of eggs and avocado or a shake with healthy fats and protein for breakfast negatively affects your liver and blood sugar. The effects may be less dramatic for some (those with a healthy weight and insulin sensitivity) and accelerate the negative effects for those that are overweight or prediabetic. A perpetual cycle of overeating chokes the liver and creates the perfect environment for systemic inflammation, high triglycerides (TAGs), elevated LDL- particle number, leptin resistance, dyslipidemia, and insulin resistance.
Having a clogged liver is serious business. The liver is responsible for detoxifying the body. In today’s world it is under constant assault from toxicants. In addition to the liver’s detox duties it plays a large role in the conversion of fuel to energy. An overloaded liver creates a slow metabolism. Even worse it fails to recognize insulin signaling and continues to unload sugar into the blood stream. When your liver is struggling and you consume a high carb meal it is estimated that 80% of the sugar in the blood stream has its origin in the liver and not a spike from recently consumed food.
If your liver is clogged it may continue down four stages of disease progression:
NAFL - nonalcoholic fatty liver
NASH - nonalcoholic steatohepatitis
Fibrosis - inflammation causes scar tissue
Cirrhosis - function impaired and can be life threatening
Eat the standard American diet for 5 years and chances are you may fit the criteria for Metabolic syndrome (MetS). MetS comes with a host of risk factors including cardiovascular risk. Click here to read more about the risk of cardiovascular disease.
Abusing stimulants such as caffeine can disconnect you from your natural circadian rhythm and disrupt cortisol patterns. Some people are better at metabolizing caffeine than others. Alcohol in excess can hijack restorative sleep and boost cortisol as well. Everyone is different and women typically produce less alcohol dehydrogenase that breaks down ethanol into acetaldehyde. If you have heard of alcohol flush this is due to accumulation of acetaldehyde and deficiency in aldehyde dehydrogenase 2. The point is you are taxing your metabolic resources.
3.Gut problems
If you are having gut issues, with intestinal symptoms or not, your metabolism and hormonal health may suffer. The renewed interest in our microbiome is a breath of fresh air. The microbes that inhabit the human GI tract play a role in human health and disease. For a tube whose contents are actually outside the body it plays a role in nutrition, digestion, immune processes, the central nervous system and energy homeostasis.
The disruption of the microbiome-gut-brain axis has a wide array of implications. You may be familiar with the term “leaky gut”, irritable bowel syndrome, metabolic endotoxemia or small intestinal bacterial overgrowth (SIBO). Those that have intestinal permeability or a leaky gut may develop food intolerance and fat loss resistance. Give the book Wheat Belly or The Plant Paradox a read if you want to learn more. For those that want the deep dive check out The Mind-Gut Connection.
When the microbiome is restored to a healthy set-point it trains and regulates our immune system. It keeps gut inflammation at manageable levels, limits pathogenic growth, helps prevent allergies, reduces gas and has anti-tumor properties. You may not be aware that 20-25% of T4 is converted to T3 (active thyroid hormone) in the gut.
What can disrupt the gut:
Medications (PPI’s, antibiotics, Birth control, corticosteroids)
Wheat/gluten/lectins
Alcohol and high sugar intake
Parasites and infection
Low stomach acid
Poor intestinal motility
Sleep and Stress
4.Stress and sleep debt
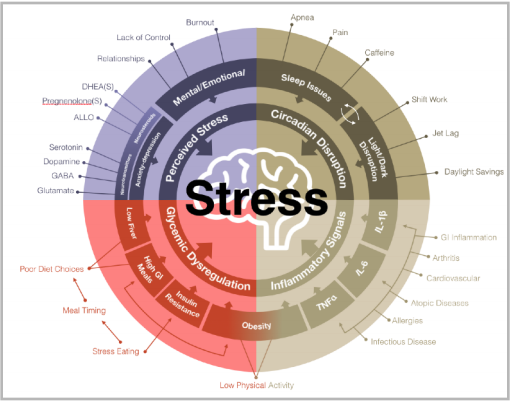
When we are stressed our brain knows. Specifically the HPA axis (hypothalamus, pituitary and adrenals) is busy preparing the body to adapt to the four types of stress:
Perceived stress e.g.mental/emotional and anxiety and depression)
Inflammatory signals e.g. GI, allergies or cardiovascular signals
Glycemic dysregulation e.g.insulin resistance and obesity
Circadian disruption e.g sleep issues (pain/apnea) or light dark disruption
When we experience stress that lasts for weeks and months chronic levels of high cortisol are stuck in the redline position. There is evidence that chronic stress changes food preferences and leads to insulin resistance. Some researchers have found that people with sleep disturbances, high stress, depressed mood and anxiety are strong predictors of low back pain.
A good night’s sleep will improve glucose metabolism, boost growth hormone secretion, and help normalize and help regulate cortisol levels. Because cortisol is released in a rhythmic fashion it’s not uncommon to see dysfunctional 24 hour cortisol patterns. This can contribute to fatigue throughout the day and difficulty sleeping in the evening. For example if a person has a disrupted cortisol rhythm but otherwise normal cortisol production symptoms may include fatigue, sleep disturbances, and higher perceived stress.
5.Excess Inflammation
Inflammation is a normal response to injury. We rely on inflammation to signal the immune system for cell injury and repair or defend us against bacterial or viral infections. When inflammation becomes chronic - metabolic disease begins to take hold.
Inflammation may be the most important mechanism driving “diabesity” (the one-two punch of diabetes and obesity). Elevated inflammatory markers are predictive of weight gain and insulin resistance. Those with higher levels of inflammatory cytokines and liver inflammation have an increased risk for diabetes. Inflammation of the brain leads to leptin resistance. Women suffering from endometriosis may be surprised to learn that it is best defined as an inflammatory disease. Are you beginning to see why we want to minimize nonessential levels of inflammation?
Food allergies are quite different than food intolerances. Many Americans have food intolerances and unknowingly consume these foods. For example men and women respond differently to grains when it comes metabolic dysregulation. Some may be completely free of intestinal issues while other exhibit a constellation of symptoms such as a thick waist, abnormal cholesterol, high blood pressure, and or problems with blood glucose. Because you need special enzymes to break down gluten, a protein found in wheat and grains, some researchers think that up to 80% of the population lack the necessary enzymes to properly digest gluten. Dairy sensitivity is also common however it seem more problematic when patients have a leaky gut, dysbiosis and consume low-fat non organic dairy products.
In the 90’s we were told to eat more grains and cut the fat. According to the CDC the diagnosis of diabetes has tripled. Even more concerning is the increasing trend in autoimmune disease in general. This includes Hashimoto’s/ Graves disease, Sjogren’s, irritable bowel disease (IBD), rheumatoid arthritis , lupus and celiac’s disease. The unsettling truth is that these autoimmune diseases are on the rise and in some cases are 2-3 times more common than a few decades ago. Experts believe that symptoms of autoimmune disease may be prevented by re-establishing intestinal barrier function.
An improper diet can lead to increased levels of inflammation. This includes diets low in calories i.e. 40% or greater caloric deficits over a 6 week period. Diets that lack comprehensive nutrient profiles such as veganism, fruitarian or vegetarianism are at higher risk of elevated inflammation in the long term.
6.Too much or too little exercise
Regaining metabolic flexibility is directly tied to your diet. Too much exercise, with a sluggish metabolism, is a big stressor. This is especially true if your performing long workouts on a low calorie diet. However, the right amount of exercise can provide some amazing benefits including increased insulin sensitivity, fuel expenditure, muscle health, glycogen production and mitochondrial health. If you are too sedentary and maintain a poor diet your muscles atrophy and you body composition will creep to higher fat and lower % of lean muscle. When that happens your resting metabolism slows down.
It’s very important that you sort out your “chemistry” before exercise is able help you in maintaining a healthy weight. Don’t forget your liver has to process all the calories and fuel you burn up during exercise.
7.Hormone imbalance
Whether you have adrenal fatigue, more correctly referred to as HPA axis dysregulation, excess estrogen, low testosterone, PCOS or diabetes it alters your metabolic machinery. That new metabolism you’re fighting for through diet and lifestyle changes will seem recalcitrant.
Books are written on this topic so let’s touch on the thyroid since it’s a major player in regulating your metabolism, and assuring good general health. Most people wrestling with weight need to address their relationship with grains. In addition to providing high amounts of calories they may lead to intestinal permeability and the body’s immune system attacking itself. For example, people with Hashimoto’s disease are usually put on thyroid hormones. Dr. Kresser uses an analogy of bailing water.
People with low thyroid may need thyroid hormone as a necessary part of the treatment. But unless the immune dysregulation is addressed (plugging the leaks), whoever is in that boat will be fighting a losing battle to keep it from sinking. Meanwhile, that person will struggle with weight loss resistance.
8.Ignoring key body measurements
Time to move away from BMI as it’s not as predictive as other measurements. Waist circumference (WC), waist-to-hip ratio (WHR) and waist-to-stature ratio have larger effects on increased CVD risk compared with body mass index (BMI).
For most of us we get an up close look of our bodies in the shower and when we are dressing. Measurements looking at central obesity, fat deposits in the abdomen, and around the viscera organs are better independent predictors of cardiovascular disease, fatty liver and diabetes.
9.Not testing basic biomarkers
Looking at the blood is an imperfect proxy, but it is one of the better ways to see whats going on under the metabolic hood. Below is a list of biomarkers that I would recommend for a baseline functional medicine workup.
CBC with differential
CMP (includes liver enzymes)
Fasting blood glucose, fasting insulin and HgA1C
Homocysteine
NMR lipoprofile
Full thyroid panel ( TSH , T4 reverse T3, w/Antibodies)
Perhaps a Urinary DPD (assesses bone resorption rates)
Earlier in the article I mentioned Metabolic syndrome or MetS. So what is MetS? The criteria have changed over the years, but here is the general consensus.
ANY three of the 5 Criteria below:
Obesity -- Waist circumference >40 inches for male and >35 inches for females
Hyperglycemia -- Fasting glucose ≥ 100 mg/dl or pharmacologic treatment
Dyslipidemia – Trigylcerides ≥ 150 mg/dl or pharmacologic treatment
Dyslipidemia (separate criteria) – HDL cholesterol < 40md/dl male, < 50 mg/dl females; or pharmacologic treatment
Hypertension -- >130 mmHg systolic or > 85 diastolic or pharmacologic treatment.
*Note: LDL particle (LDL-P) number appears to be the most accurate marker for predicting metabolic syndrome. How do you test LDL-P. A test called NMR lipoprofile.
If you have questions regarding any of the topics covered in this article email them to nick@spineandjointoc.com